When is it enough?
When is the suffering of patients enough? I asked myself this question after seeing patient X. To provide a background, patient X is 86 years old and was diagnosed with lung cancer, with metastasis to the throat. Over the last 5 years the patient has had a right lung pneumonectomy and a total laryngectomy, through that period the patient has had hyperthyroidism,hypertension and lately he had a CVA that led to right side hemiplegia. In addition, he has been queried for hepatocellular carcinoma. Currently, he has a huge sacral pressure sore that started developing 3 years ago. The patient is taking a long list of medications for the cancer, hypertension and for the excruciating pain he is experiencing. To make matters worse, some of these drugs are giving him side effects. Functionally, the patient is unable to do anything. He is being fed via a nasogastric tube and cannot speak or move any of the limbs. The only way for him to communicate or provide feedback is though blinking, facial expressions and sometimes through mouthing words.
It is the experience of this patient that led me to believe that it is their right to decide what they must do with their lives. Legally, the right of a competent, terminally ill person to avoid excruciating pain and embrace a timely and dignified death bears the sanction of history and is implicit in the concept of ordered liberty. The exercise of this right is as central to personal autonomy and bodily integrity as rights safeguarded by this country’s constitution on decisions relating to marriage, family relationships, procreation, contraception, child rearing and the refusal or termination of life-saving medical treatment.
I fully understand that as a health practitioner my role is to improve the quality of life of the patients that I treat, Ironically the aforementioned sentence mentions “improving quality of life” which is a very subjective matter. Surely, from person to person the idea of quality of life differs either by small or bigger margins. Yes, there are common baselines such as physical functioning, social functioning, mental functioning etc. as the study by J Hofhuis et al(2015). But all these can never accurately reflect everyone’s quality of life, and there is this idea of patient centred care which is even endorsed by the World Health Organization, which focuses on the patient and the individual’s particular health care needs. The goal of patient-centred health care is to empower patients to become active participants in their care and to be addressed holistically (Lusk & Fater, 2013). Which leads me to a belief that as health practitioners, serving patients best interest should be our fundamental role and even if they want to take their lives.
To explore this topic in a South African context, Its important to acknowledge that our sphere consists of complex interactions between religion, culture and legal aspects that dictate the state of our affairs. However, I will be focusing more on the legal aspect as I can use the constitution as a reference. Our law defines murder according to these following instances.
- Murder consists in the unlawful and intentional killing of another human being.
- Attempted Murder consists in the commission of an unlawful act with the intention of
killing another human being but which does not result in the death of that human
being. - Culpable Homicide consists of the unlawful, negligent causing of death of another
human being.
As you can see above, our law doesn’t necessarily say anything about assisted suicide, which leaves a grey area that gave rise to Stransham-Ford case, who requested legal permission from the Gauteng North High Court (of 29 April 2015) to have medical doctors help him to end his life due to unbearable suffering from his terminal illness. (Evanns, 2019) He did acquire the permission to go ahead, even though the High Court decision was later heavily criticized by the National Minister of Health, Dr Aaron Motsoaledi; the South African Catholic Bishops’ Conference, the Department of Justice and Correctional Service ; and other religious movements as well as the Health Professions Council of South Africa (Evanns, 2019) . This suggests that there is a need of constitution restructuring to accommodate this topic, and for that to happen foundations like Dignity SA, that is found by Sean Davison, who is currently going through a trial for assisting his friends to end their suffering on their request (Evanns, 2019) . These foundations can play a huge role into bringing this topic into the public light and that may lead to a parliamentary discussion which may lead to a possible constitutional change to accommodate euthanasia.
For the latter to happen, a rigorous process must be followed. This process should include thorough consultation of all stakeholders involved from the medical team, family members and legal teams if necessary. They all must be satisfied that the patient’s request is voluntary and well-considered, secondly, they must be satisfied that the patient’s suffering is unbearable and that there is no prospect of improvement, thirdly, they must inform the patient of his or her situation and further prognosis, and finally they must discuss the situation with the patient and come to the joint conclusion that there is no other reasonable solution (Visser, 2019). 3 paragraphs can never do justice this topic, however in closing, In South Africa The Stransham-Ford case is valuable in the sense that it has allowed for euthanasia to be robustly and openly debated in legal, political, religious, cultural and sociological fora. The Judgement of the Gauteng North High Court in the same case suggests that individual instances of euthanasia should be decided on a case-by-case basis: in this way, there would be no one-size-fits-all policy on such a matter. I argue that the value of moral decisions is viewed on the basis of how well they serve persons in their unique situations. The ability of humankind to make rational decisions on complex, sensitive issues is largely dependent on the existence of a culture of debate in which different points of view are put forward and considered. Such a culture would enable citizens to develop and defend their opinions, based on whatever value system they choose to adopt. The sooner moral issues and applied ethics are introduced into the South African education system and continued throughout higher education, the better prepared citizens will be to participate in policy-making decisions in this country.
REFERENCES
The South African. (2019). Assisted Dying: South African law and the right to die on your terms.
[online]
Available at:
Assisted Dying: South African law and the right to die on your terms[Accessed 9 Jun. 2019].
Hofhuis, J., Stel, H., Schrijvers, A., Rommes, J., & Spronk, P. (2015). Recovery of health-related quality of life in ICU patients: a 5-year prospective cohort study. Critical Care, 19(Suppl 1), P565. doi: 10.1186/cc14645
Lusk, J., & Fater, K. (2013). A Concept Analysis of Patient-Centered Care. Nursing Forum, 48(2), 89-98. doi: 10.1111/nuf.12019
Visser, D. (2019). Euthanasia, assisted suicide and non-resuscitation on request. Retrieved from https://www.government.nl/topics/euthanasia/euthanasia-assisted-suicide-and-non-resuscitation-on-request
Evanns, J. (2019). Euthanasia advocate Sean Davison has bail extended after case postponed.
[online]
News24. Available at: https://www.news24.com/SouthAfrica/News/euthanasia-advocate-sean-davison-has-bail-extended-after-case-postponed-20190129 [Accessed 9 Jun. 2019].
4 thoughts on “When is it Enough”
Hi Andile,
Thanks for sharing your writing. I am going to give feedback following the rubric so its easy to follow and has some structure.
Substance/Content: I am not quite sure of the topic you are addressing, I am guessing it is euthanasia and/or meaningful life/death. I think you can make this more clear in your writing, it will then be easier for the reader to understand claims /statements and how/why you justify them. Once this is more clear I think you can provide more in-depth information on the topic and draw effectively on references appropriate. I think you have made an original contribution, I like that you described your personal experience first-this gave me insight as to why you chose to write this and provided me with a mental image to work with while reading. I think you once you are clear about your topic, your content will be more easily understood and flow nicely- try to stick with one idea per paragraph. For each of these, provide claims and substantiate these with adequate evidence.
Synthesis of content/discussion/reflection/critical thought: I think your ideas blend well with the coursework and ideas/topics we have discussed in class but as I have said above you can be more clear as to which topic you are addressing. Perhaps once you have done this you can draw on ideas of similar previous posts by students? I think you have demonstrated some critical thinking and analysis but with more research and evidence this will be enhanced. I think because your topic is not clear, the writing stays on a ‘knowledge’ level and is predictable, once you are clear on your topic and consequently researching within the realm of the topic your writing will more into stronger critical thinking.
Engagement: I think this section of the rubric is more how you engage with other students/feedback but with regards to this piece, I think you can engage more with your experience and with evidence. I suggest reading articles on legalities, views and other experiences and also looking at the reference lists of these articles.
Writing Style: there is spelling and grammatical errors, I will try help with this in another comment. I know English is not your first language so I salute you for writing this. Despite this, I see you have a strong writing style and think it can only flourish with clearer topics and reading.
References: you have included references and these are correctly referenced. As I said before, I think you can build on this reference list to make more concrete and new views.
Time/length: I think your piece can be longer, you can delve into more ideas and concepts and provide more evidence to claims.
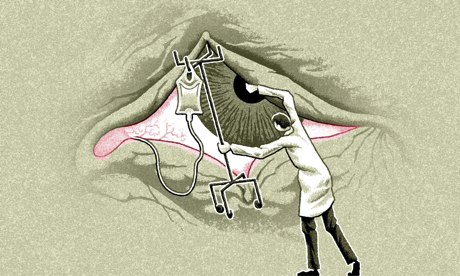
Information literacy: perhaps you can add a picture or video or something to stimulate the reader regarding your idea/topic. Add this as a featured image.
Well done!
I look forward to reading the updated version.
Jemma
Spelling and grammar corrections:
When is it enough?
When is the suffering of patients enough? I asked myself this question after seeing patient X. To provide a background, patient X is 86 years old and was diagnosed with lung cancer, with metastasis to the throat. Over the last 5 years the patient has had a right lung pneumonectomy and a total laryngectomy, through that period the patient has had hyperthyroidism,hypertension and lately he had a CVA that led to right side hemiplegia. In addition, he has been queried for hepatocellular carcinoma. Currently, he has a huge sacral pressure sore that started developing 3 years ago. The patient is taking a long list of medications for the cancer, hypertension and for the excruciating pain he is experiencing. To make matters worse, some of these drugs are giving him side effects. Functionally, the patient is unable to do anything. He is being fed via a nasogastric tube and cannot speak or move any of the limbs. The only way for him to communicate or provide feedback is though blinking, facial expressions and sometimes through mouthing words.
It is the experience of this patient that led me to believe that it is their right to decide what they must do with their lives. Legally, the right of a competent, terminally ill person to avoid excruciating pain and embrace a timely and dignified death bears the sanction of history and is implicit in the concept of ordered liberty. The exercise of this right is as central to personal autonomy and bodily integrity as rights safeguarded by this country’s constitution on decisions relating to marriage, family relationships, procreation, contraception, child rearing and the refusal or termination of life-saving medical treatment.
I fully understand that as a health practitioner my role is to improve the quality of life of the patients that I treat, Ironically the aforementioned sentence mentions “improving quality of life” which is a very subjective matter. Surely, from person to person the idea of quality of life differs either by small or bigger margins. Yes, there are common baselines such as physical functioning, social functioning, mental functioning etc. as the study by J Hofhuis et al(2015). But all these can never accurately reflect everyone’s quality of life, and there is this idea of patient centred care which is even endorsed by the World Health Organization, which focuses on the patient and the individual’s particular health care needs. The goal of patient-centred health care is to empower patients to become active participants in their care and to be addressed holistically (Lusk & Fater, 2013). Which leads me to a belief that as health practitioners, serving patients best interest should be our fundamental role and even if they want to take their lives.
For the latter to happen, a rigorous process must be followed. This process should include thorough consultation of all stakeholders involved from the medical team, family members and legal teams if necessary. They all must be satisfied that the patient’s request is voluntary and well-considered, secondly, they must be satisfied that the patient’s suffering is unbearable and that there is no prospect of improvement, thirdly, they must inform the patient of his or her situation and further prognosis, and finally they must discuss the situation with the patient and come to the joint conclusion that there is no other reasonable solution (Visser, 2019). 3 paragraphs can never do justice this topic, however in closing, the option for patients to terminate their lives when they had enough suffering should be always available for them.
Hi Andile
Thank you for sharing your piece and your experience with this particular patient. It is quite a heartbreaking situation that the patient had to endure.
Please have a look at paragraphs one ,two and three as there are a few grammatical errors. I like the way in which you provide the background of your patient and move on to introducing the concept of euthanasia. I liked the way in which you addressed the process that needs to be followed should a patient avoid further medical treatment, it provides the reader with a process they may potentially follow should they find themselves in a situation where they patient no longer wishes to receive medical treatment. Have you perhaps considered exploring the concept of euthanasia a bit more in depth before making your way to the processes that need to be followed should a patient no longer want medical treatment ? In addition , it may helpful to explore the concept of euthanasia within South Africa and having a look at the laws surrounding it. Good referencing, however it would be helpful if you make use of more literature. Literature focusing on the concept of euthanasia within South Africa and the laws surrounding this particular concept as well. Well done, Andile ! I’m looking forward to your final piece !
Hi Andile.
Thanks for sharing this piece for me to read.
In terms of the context as well as your topic,I am not sure which topic you’re trying to address; is it meaningful life/meaningful death or euthanasia?
Your content makes clear links to both of the above leading to the confusion.
Your piece links more to euthanasia so I’m taking it upon myself to assume that’s what you’re looking at.
You explored the topic well but I do think there is room for more referencing to back up some claims and that you could possibly delve more into when the choice is made,is it legal and/or ethical and who has the right to make this choice.
Perhaps explore the South African context as well as the physiotherapy context in terms of when treatment is terminated,the effect of the choice on treatment and would it be legal or ethical for the physiotherapist to terminate treatment.
Your content had a flow and each paragraph linked to the next but as I said,there is room to expand on it and lengthen this piece.
Your references are correct.
Thank you and good luck.