During my general block, I was working with a 79-year-old male patient. The patient had been admitted due to a sudden change in gait, which was suggestive of possible neurological involvement. The patient was also delirious, secondary to a Urinary Tract Infection (UTI). After a CT Brain, it was determined that there was no neurological involvement. The patient presented with a slight scissor gait and poor balance and thus was unable to mobilize independently. The patient’s UTI resolved but his delirium did not improve. The patient was often disorientated, although the degree of his confusion varied daily. Some days the patient was able to report that he was in a hospital and that he wanted to go home to his family. Other days, the patient was in a different time-period and would report that he was still living with his parents and that he has two young children, when in fact he lives with his adult son. He would also refer to objects that were falling from the roof. Doctors were trying to ascertain if the patient had dementia. The patient did progress physically as he regained some strength and was able to mobilize with moderate assistance from two physiotherapists.
The patient’s demeanor during my treatment sessions was very calm and respectful. Whilst he was confused with regards to place and time, he was still able to follow my instructions and was responsive to assistance. Due to my experiences with this patient, I was therefore very surprised when I arrived at my patient one day to find him physically restrained. When I enquired with the nursing sister as to why this had been done, she reported that the patient had attempted to climb out of his high cot bed and was at risk of falling, especially as he is unable to mobilize independently.
This confused me as from what I had experienced with this patient, I did not think this was in line with his usual character. I thus faced this ethical dilemma of whether I agree with patients being restrained, especially with patients who do not have the capacity to understand why they are being restrained.
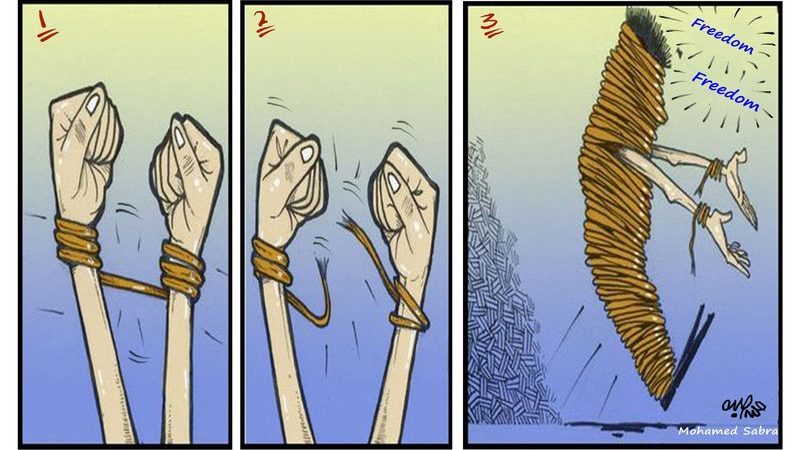
Patient Autonomy is defined as “The right of patients to make decisions about their medical care without their health care provider trying to influence the decision. Patient autonomy does allow for health care providers to educate the patient but does not allow the health care provider to make the decision for the patient” (Ye, 2018). The use of physical restraints violates the principle of autonomy because it breaches the freedom of patients; hence, such a practice is then actually considered unlawful (Ye, 2018). Yet this still occurs daily in many South African hospitals.
A recent study conducted in South Africa showed a prevalence of 23% of patients being restrained (Kalula, 2016). An alarming result from this study showed that the majority of nurses and doctors reported that no consent was obtained from patients or a family or legal representative before the restraint was used (Kalula, 2016). According to the Health Professionals Council of South Africa, The National Health Act of South Africa sets out a priority list of persons whom are who may consent on behalf of mentally incompetent patients: It may either be a person authorized by the court (e.g. a curator); or, in order of priority, the patient’s spouse, partner, parent, grandparent, major child, brother or sister. Therefore when a patient is restrained, it is actually legally required that an authorized person be contacted before restraining the patient.
A restrained patient is unable to provide for his or her basic needs, which include turning, eating, drinking and toileting (Maccioli, 2003). Health professionals who care for restrained patients must therefore be skilled in providing for these needs, while simultaneously monitoring the patient for complications arising from restraint (Maccioli, 2003). But nurses working in South African hospitals are already inundated with the amount of work they are required to do due to insufficient staffing, and thus it is difficult to provide this specialized care that a restrained patient should be receiving. In South Africa some hospitals have ratios that go as high as one nurse for every 18 patients (Solidarity Research Institute, 2009). This results in a nurse having only three minutes per hour to care for each patient, to perform all routine tasks (Solidarity Research Institute, 2009), therefore this specialized care for restrained patients is not always possible.
My view regarding restraining patients is conflicted as I believe prisoners should be restrained as their freedom of movement should be limited based on the fact they have been convicted of a crime and thus may be a danger to other people around them. The definition of physical restraints states that they are “Devices and practices that restrict a patient’s movement” (Lane, 2011). Therefore, by restraining other patients, I believe we are treating them like prisoners and removing their freedom of movement. According to the Bill of Rights, Chapter 2 of the Constitution of the Republic of South Africa, everyone has the right to bodily and psychological integrity, which includes the right to security in and control over their body. The use of physical restraints directly infringes on the patient’s freedom of the control over their body, therefore indicating that physically restraining a patient is in fact a violation of their human rights.
However, I also understand that if a patient is unable to comprehend their impairments, then they do need to be restrained in order to prevent falls, otherwise they are a danger to themselves. Nevertheless, I do still feel that an increased amount of patients are being restrained in South African hospitals due to insufficient staff and thus there are not enough nurses to monitor all of the patients, therefore to prevent any incidents, restraining patients becomes the easier option.
When I continued to treat my patient, I would remove the patient’s restraints during our session, but I was required to restrain him again afterwards as the nursing sister was afraid he would fall if left unsupervised. Whilst the patient had not complained about the restraints, I was concerned that one day he could wake up and become anxious when he sees the restraints and not be able to understand the reason for the restraints and this could worsen his already disorientated mental state.
I only truly understood the nursing sister’s concern when I witnessed this patient attempting to climb out of his high cot bed. Whilst I was not treating this patient at this particular time, I was in the same ward as him. His ankle restraints were not on at this moment and as I walked past him, he was hooking his legs over the cot-side and attempting to climb out. When I asked him what he was doing, he reported he was leaving to go and fetch his son from school. It was in this moment that I realized that due to his inability to make rational decisions and lacked understanding of his condition; he was truly a danger to himself. In this scenario, I can then understand why restraining this patient is necessary even though the patient’s right to freedom of movement is now in question as a result of his impaired lack of judgment.
If I were placed in a similar position in in the future, I would still query with the nursing staff as to why the patient has been restrained, as I still do believe restraining patients should be kept to a minimum if possible. I would however also consult with the doctor, and any other health professionals who are also attending to the patient to get their view of the patient’s demeanor in order to assess if the restraints are necessary. Thereafter rather discuss the need for the restraints as a Multidisciplinary Team so that the responsibility of the decision-making process regarding restraining patients is not solely dependent on the nursing sister in charge.
References:
Kalula, S. Z., & Petros, S. G. (2016). Use of physical restraint in hospital patients: A descriptive study in a tertiary hospital in South Africa. Curationis, 39(1), 1-8.
Lane, C. & Harrington, A., 2011, ‘The factors that influence nurses’ use of physical restraints: A thematic literature review’, International Journal of Nursing Practice 17(2), 195-204.
Maccioli, G.A., Dorman, T., Brown, B.R., Mazuski, J.E., McLean, B.A., Kuszaj, J.M. et al., 2003, ‘Clinical practice guidelines for the maintenance of patient physical safety in the intensive care unit: Use of restraining therapies – American College of Critical Care Medicine Task Force 2001-2002’, Critical Care Medicine 31, 2665-2676.
Ye, J., Xiao, A., Yu, L., Wei, H., Wang, C., & Luo, T. (2018). Physical restraints: An ethical dilemma in mental health services in China. International journal of nursing sciences,5(1), 68-71.
Solidarity Research Institute. May 2009. Nurse shortage in South Africa: Nurse/Patient ratios. Retrieved from https://cisp.cachefly.net/assets/articles/attachments/21373_solidarity.pdf
The Healthcare Professionals Council of South Africa. 2008. Seeking patients’ informed consent: The ethical considerations. Booklet 9. Pretoria Retrieved from https://www.hpcsa.co.za/downloads/conduct_ethics/rules/generic_ethical_rules/booklet_9_informed_consent.pdf
Bill of Rights. 1996. Chapter 2 of the Constitution of the Republic of South Africa. Retrieved from https://www.westerncape.gov.za/legislation/bill-rights-chapter-2-constitution-republic-south-africa#12
2 thoughts on “Patients or Prisoners?”
Hello Halinka,
Thank you for allowing me to read your piece on Patients or Prisoners. I enjoyed reading your piece and gaining more insight to what this topic means to you. Your writing piece reflects on the topic’s discus in the class. Therefore, I would rate your content as good. I liked how you explained why you believe patients should not be treated as prisoners and be restrained. The argument you made against and for restrains was very well explained. It is a very difficult to restrain a patient when you have been treating the patient and when you know that the patient does not need restrains. Your writing piece made me think of my own clinical practice and what I would have done in this situation. I like that you added a South African context to your piece and touching on insufficient staff. Perhaps you can add more context to your piece by referring to other reasons why patients’ get treated like prisoners in South Africa.
I liked the argument that you made about why patients should not be restrained. I agree that patients should be allowed their freedom of movement as they are not prisoners. Perhaps you can make your argument stronger by adding more to the part where you talk about South African hospitals having insufficient nursing staff. Due to the insufficient nursing staff the patients that are restrained are often just left in bed and when they try to get the nursing staffs attention they are seen as difficult patients. This just adds to the feeling of being in prison. Your counterargument was well made. I can understand why you are conflicted about restrains.
Adding references to the writing piece will make your argument stronger. Remember to add in-text referencing as well as your reference list at the bottom of your writing piece. To make your writing piece stronger try to get references from both sides of the argument.
Few grammar errors that I have noticed:
Fourth paragraph
• Fourth sentence – Change amount to number
Fifth paragraph
• First sentence – Add , after afraid
Sixth paragraph
• Third sentence – Change was to were. “His ankle restraints were”
Overall, your writing piece touches on a real ethical dilemma that many people will have conflicting opinions on. The paragraphs were well constructed and easy to read. I hoped my comments are going to be of good use.
Good luck with your final
Megan
Hi Halinka!
Thank you for your piece. This is a very relatable topic. I myself have had a patient similar to this and I too struggled to understand why they restrained my patient.
Your piece has good statements and is very relatable as you included how you feel about the situation. This helps the reader connect to your writing. I like that you included why you think your patient was restrained and what the nurses says. It shows the apposing views very well, and how you changed your opinion when you saw how unsafe the patient was.
Maybe just add some literature to back up some of your statements and a picture to help relate to your piece.
Overall a very well written piece!
Thanks, Sonali xx